Employee eligibility

Determining employee, dependent eligibility
An eligible employee is a person who:
- you employ on a permanent, full-time basis for the required number of hours per week as shown in your current Dean Health Plan Employer Group Master Policy;
- is an employee you identify as someone who must be covered pursuant to the Patient Protection and Affordable Care Act.
See your Group Master Policy for the eligibility statement for your group.
 View Sample Group Master Policy
View Sample Group Master Policy
Learn more about enrolling your employees
 Probationary period
Probationary period
Newly hired, eligible employees and their dependents are eligible for coverage after serving the probationary period established by your group and listed in your Group Master Policy.
To change the probationary period, you must notify your Account Manager in writing before the date of the change. The probationary period cannot extend beyond 90 days.
Note: coverage for the eligible employee and any qualified dependents may not become effective if the eligible employee is not actively at work on the effective date. See your Member Certificate for further details.
Employees and their dependents who initially waived coverage may be eligible for benefits later due to a qualified status change or event. See our Qualifying Events Guidelines for more information.
 Plan type eligibility
Plan type eligibility
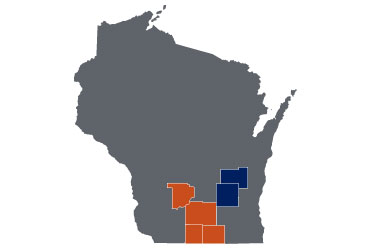
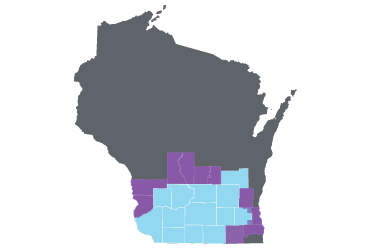
If your group offers PPO and/or POS segments, the following employees are eligible to enroll in those segments:
- All benefit-eligible employees may enroll in the HMO or POS segment if they either live or work in our service area
- Employees who live outside Wisconsin or outside the Dean Health Plan service area may enroll in the PPO segment. Members may be eligible for the PPO product based on their resident ZIP code.
 Dependent eligibility
Dependent eligibility
An eligible dependent is defined as the subscriber's:
- Legally married spouse, domestic partner*, biological child, adopted child, child placed for adoption and/or stepchild to the end of the month the dependent turns age 26. *Not all group plans cover domestic partners. See your Group Master Policy.
- Dependent under age 26 who is called to active duty. He or she can be reinstated to the parent’s plan upon return from active duty.
- Dependent age 26 or older who was called to active duty prior to reaching age 27. He or she can be reinstated to the parents’ plan if he or she was a full-time student before military service and re-enrolls as a full-time student after military service.
- Biological child of an unmarried dependent child until the dependent child (who is also covered as a dependent) is age 18. Coverage for the child of the dependent will be terminated on the dependent’s 18th birthday.
If the subscriber’s dependent is disabled, coverage may be available beyond age 26. To qualify as disabled, a subscriber’s dependent must be approved by the Underwriting Department. See your Member Certificate for definition of disabled dependent.
Eligibility resources
Eligibility file
If you have 51 or more employees, or you use a third-party administrator for benefits enrollment, you may consider sending us a HIPAA-compliant Electronic Enrollment Transaction (834) in lieu of Employee Application for Group Coverage forms. If your group is interested in sending electronic enrollment transactions, contact your Account Manager to get started or read more about 834 transactions on the Employee-Enrollment page.